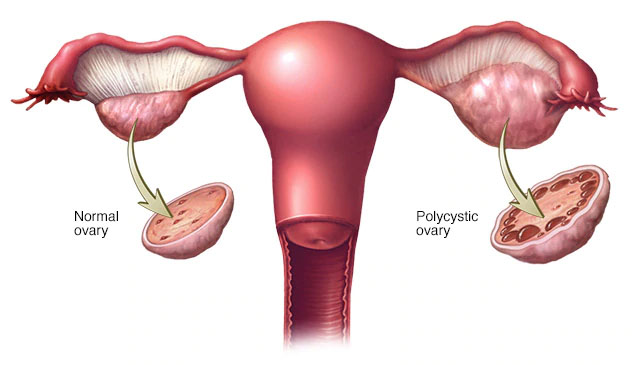
Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) affects 12-18% of women of reproductive
age and up to 21% in some high-risk groups, such as Indigenous women. In
these pages you will learn all about the signs and symptoms of PCOS, how it
is diagnosed and what treatments are available to help. There is information
on PCOS and irregular periods, acne, excess hair, hair loss, depression,
anxiety, sex and relationships and other health problems associated with
PCOS such as metabolic syndrome, type 2 diabetes and cardiovascular
disease.
Symptoms & causes
The symptoms of PCOS include excess hair (hirsutism), scalp hair loss, acne,
weight gain, difficulties with fertility, increased anxiety and depression and
irregular or infrequent periods. There is also information on the possible
causes of PCOS, and other health problems linked with PCOS.
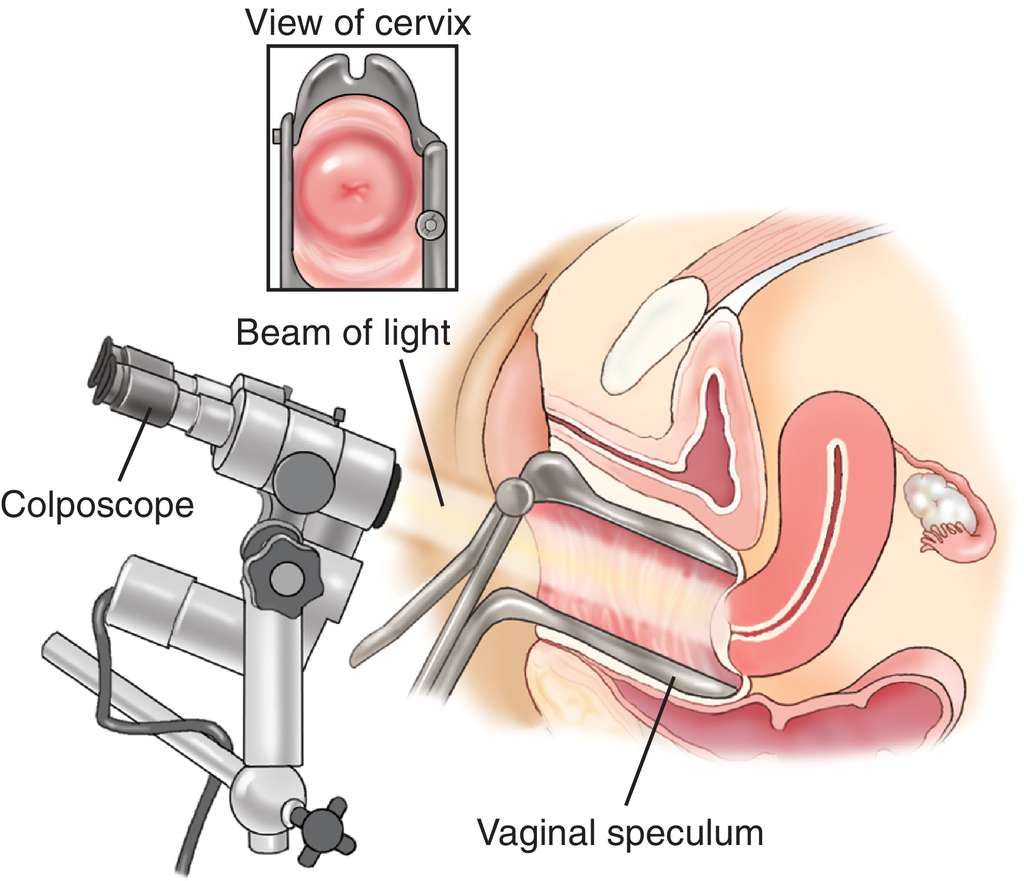
How is PCOS diagnosed?
PCOS is diagnosed by ultrasound and blood tests .
when to see your doctor and how your doctor might test you for PCOS
depends upon the clinical sins and symptoms
Management & treatment
Management and treatment of PCOS can include a range of elements such
as a healthy approach to diet and physical activity, medications and
complementary therapies.
Irregular periods - management & treatment
Irregular periods can be a symptom of PCOS. Learn about what an irregular
period is and the different ways to manage and treat irregular periods if you
have PCOS including hormonal contraception, such as the oral contraceptive
pill, and metformin.
Hair & acne - management & treatment
Excess hair, hair loss and acne are often symptoms of PCOS. Learn about
the different ways to manage these symptoms including waxing, laser hair
removal, electrolysis, hormonal contraceptives, drugs for insulin resistance
and anti-androgen drugs.
Fertility - management & treatment
Find information on the different ways to increase the likelihood of becoming
pregnant if you are having difficulties with fertility. Learn about weight and
fertility, monitoring ovulation, different medications you can try, ovulation
induction, surgery and assisted reproductive technology.
Weight - management & treatment
It can be difficult to manage your weight when you have PCOS. Below you will
find information on the influence of weight on PCOS symptoms, the benefits
of preventing weight gain and different ways to manage weight loss.
Complications
Other health problems that have been linked to PCOS include information on
prediabetes, type 2 diabetes, cardiovascular disease, metabolic syndrome
and endometrial cancer. You can also learn about BMI (body mass index) and
how to measure your BMI.